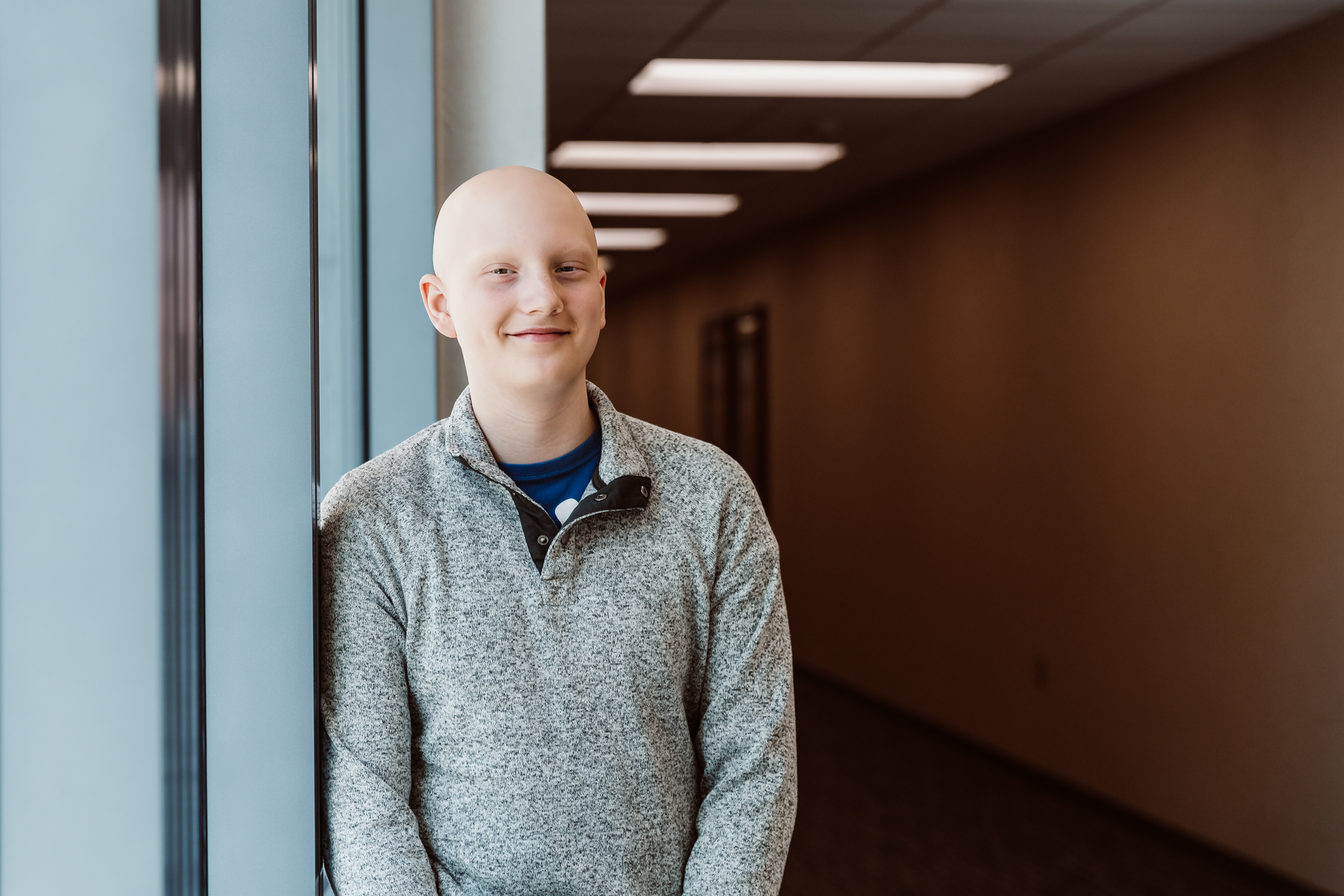
Bolton’s Bravery
With specialized, comprehensive care in hospitals tailored to the unique needs of pediatric patients, children’s hospitals help children and teens like Bolton defy the odds.

Every day, children’s hospitals help make moments possible. From providing access to the comprehensive care that children need to grow up to supporting children, teens, and their families with specialized treatment for some of the most complex illnesses. Discover more about the moments made possible by children’s hospital through patient stories from around the country.
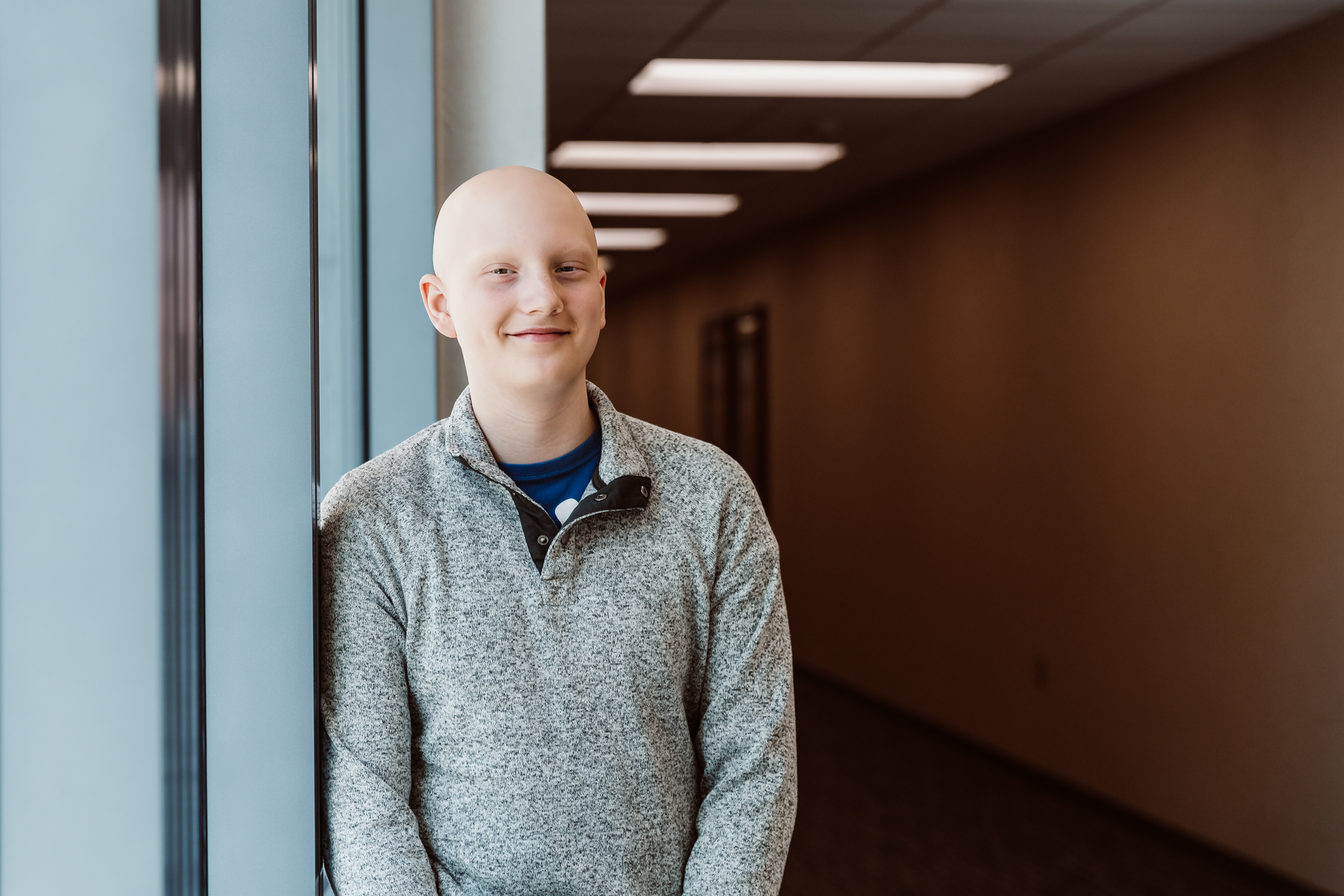
With specialized, comprehensive care in hospitals tailored to the unique needs of pediatric patients, children’s hospitals help children and teens like Bolton defy the odds.

Children’s hospitals provide advanced care for the most complex conditions in environments specially designed for pediatric patients, allowing children like Isaac to thrive.

The specialized multidisciplinary teams at children’s hospitals ensure that children and teens – like Cami – can beat multiple complex conditions like cancer and heart failure.

The advanced, specialized care that children’s hospitals provide make moments – like Joseph beating pediatric brain cancer – possible.

With care delivered by specially trained pediatric clinicians, in environments designed just for children, children’s hospitals help children and teens – like Daniella – navigate complex medical conditions.

When Sriansh was just three months old, his family grew concerned as he slept most of the day, arched his back, and could not control his eye movement. His parents brought him to Cincinnati Children’s, where he was diagnosed with AADC deficiency, a rare genetic disorder that disrupts dopamine and serotonin production in the brain. Sriansh’s family was told he might never walk, talk, or lift his head. But thanks to an experimental gene therapy clinical trial, his story took a groundbreaking turn. At just 16 months old, Sriansh became the youngest child in the world to receive a one-time gene therapy treatment, delivered directly into the brain through a minimally invasive surgical technique. His care team inserted an engineered virus carrying the missing gene, allowing his brain to begin producing the essential chemicals it lacked. Today, Sriansh is walking, running, and thriving because of this innovative clinical trial. This pioneering work helped lead to the first-ever FDA-approved gene therapy administered directly to the brain, offering hope for patients with rare genetic diseases once thought untreatable.

When Yanex was only nine months old, his doctor noticed a lack of developmental progress. Yanex still wasn’t trying to sit or crawl, and his movements were limited. But most notably, his physician was concerned about the shape of Yanex’s head. After an X-ray, his team at Nemours Children’s Health diagnosed him with craniosynostosis, a birth defect that causes seams between the bones in a child’s skull to close prematurely. This was preventing him from developing his mobility, leaving him very dependent on his parents. The craniofacial team followed up with multiple treatments. They first remodeled and expanded Yanex’s forehead and later expanded the back of his skull to provide enough room for his brain to grow. Yanex’s care team supported the family through both surgeries and the recovery, ensuring they fully understood each treatment and procedure. Yanex made a remarkable recovery, learning to crawl, walk, and run within seven months of the surgeries. He also began talking more as time went on. Today, Yanex is a healthy toddler who enjoys playing with his siblings!

At the end of summer, just as Theo was supposed to return to school, he instead settled in at Atrium Health Levine Children’s Hospital for a heart transplant. Being away from school and friends, Theo began to get lonely. That’s when Seacrest Studios at Levine Children’s Hospital invited him to co-host BINGO. Seacrest Studios are broadcast media centers built within children’s hospitals, giving pediatric patients the opportunity to explore different forms of media through interactive programs at children’s hospitals. Theo had so much fun during his first interaction that he returned any time he wanted to laugh or make a friend. On Theo’s 100th day at the hospital, Seacrest Studios staff surprised him by dressing up as 100-year-olds! Thanks to the upbeat, exciting environment Seacrest Studios provided, Theo made many happy memories and some friends along the way. Theo successfully received his new heart, and although his hospital stay is now over, he still stops by Seacrest Studios when he has follow-up appointments. Creative, interactive programs like Seacrest Studios help make pediatric hospital stays – no matter how short or long – more enjoyable for pediatric patients like Theo.

At 14-years-old, Abby began to experience knee pain. As a gymnast, Abby and her family chalked it up to an injury but when the pain didn’t go away, Abby got an MRI which revealed a mass in her leg. A biopsy confirmed it was osteosarcoma, a bone cancer that tends to occur in children and young adults. If the osteosarcoma is not advanced, it can be treated by removing the affected limb and undergoing chemotherapy. Abby and doctors at Norton Children’s Cancer Institute wanted to find a treatment path that offered her the most mobility and decided to perform a rotationplasty instead of a full limb amputation. The procedure involves removing the bottom of the femur, the knee and the upper tibia, and then the lower leg is rotated and attached to the femur. The ankle becomes the knee joint and patients wear a prosthetic limb on their reattached foot. Abby had her rotationplasty and is currently undergoing chemotherapy treatment at Norton Children’s. Abby’s family is no stranger to Norton Children’s. Her younger brother received a heart transplant at the hospital, and Abby recovered in one of the same rooms her brother used while in the hospital. The family is comforted knowing the care team at the hospital will treat Abby like family and remain optimistic about Abby’s journey.

Angelina was enjoying another day of fourth grade in January 2023 when she suddenly collapsed because of ventricular fibrillation (VF), a life-threatening arrhythmia that can lead to sudden cardiac arrest. School nurses quickly intervened with CPR, paramedics defibrillated her heart, and she was later flown to Children’s Nebraska’s Criss Heart Center for surgery. There, a cardiothoracic surgeon placed an implantable cardioverter-defibrillator (ICD) in Angelina’s chest. Her ICD tracks and analyzes her heart rhythm and will deliver a shock to her heart if she ever experiences an irregular, life-threatening arrhythmia again. Because of the quick response from her school nurses, paramedics and the expert team at Children’s, Angelina is healthy and back in school. Her school also achieved a Heart Safe School designation through the hospital’s Project ADAM program in May 2023, ensuring advanced preparedness for an unexpected cardiac event with automated external defibrillator (AED) and CPR training and a practiced response plan that improves safety for students, staff and community visitors alike. Now 10 years old, Angelina has since returned to her active lifestyle, playing the violin and piano and participating in basketball, volleyball and dance. She and her family feel supported and prepared for her future thanks to the care Children’s delivered.

When Rai was born, her parents immediately noticed something was wrong. Rai was born with facial deformities and a notch in her right eyelid, and she was having trouble eating and breathing. By the time she was 11 months old, her condition had worsened. Her parents brought her to CHRISTUS Children’s, where a CT scan revealed Rai had a complex vascular ring constricting her esophagus and trachea, explaining her troubles with eating and breathing. Doctors also discovered she has Goldenhar Syndrome, which caused her craniofacial abnormalities. Using innovative techniques and equipment, her medical team conducted a successful effective yet minimally invasive surgery. After the procedure, she received close monitoring in the pediatric intensive care unit to ensure a smooth recovery. Rai has shown remarkable progress and is a lively and vibrant child. She will receive cosmetic surgery for her facial abnormalities once she turns two or three years old. Looking back on their time with CHRISTUS Children’s, Rai’s parents are extremely grateful for the supportive medical team and the incredible care she received.

Athletic and energetic Brady began experiencing debilitating headaches and extreme fatigue when he was only 14 years old. His symptoms worsened, and a CT scan showed a blockage in his brain. Brady was admitted to Children’s Hospital New Orleans where doctors placed a shunt in his brain to address the blockage, and biopsied the tissue. Brady was diagnosed with a germ cell tumor called central nervous system (CNS) germinoma. Soon after his diagnosis, Brady underwent four rounds of chemotherapy to remove the germinomas. Through the intensive rounds of chemotherapy, Brady continued to get sick with strep and pneumonia, but he faced every new challenge with resilience and determination. Following his chemotherapy, Brady began daily radiation treatment for four straight weeks. Last September, thanks to the unwavering support from his family and care team, he completed radiation and rang the bell two times, signaling the end of his cancer treatment. Now, Brady is a freshman in high school, recently earning a spot on the honor roll.