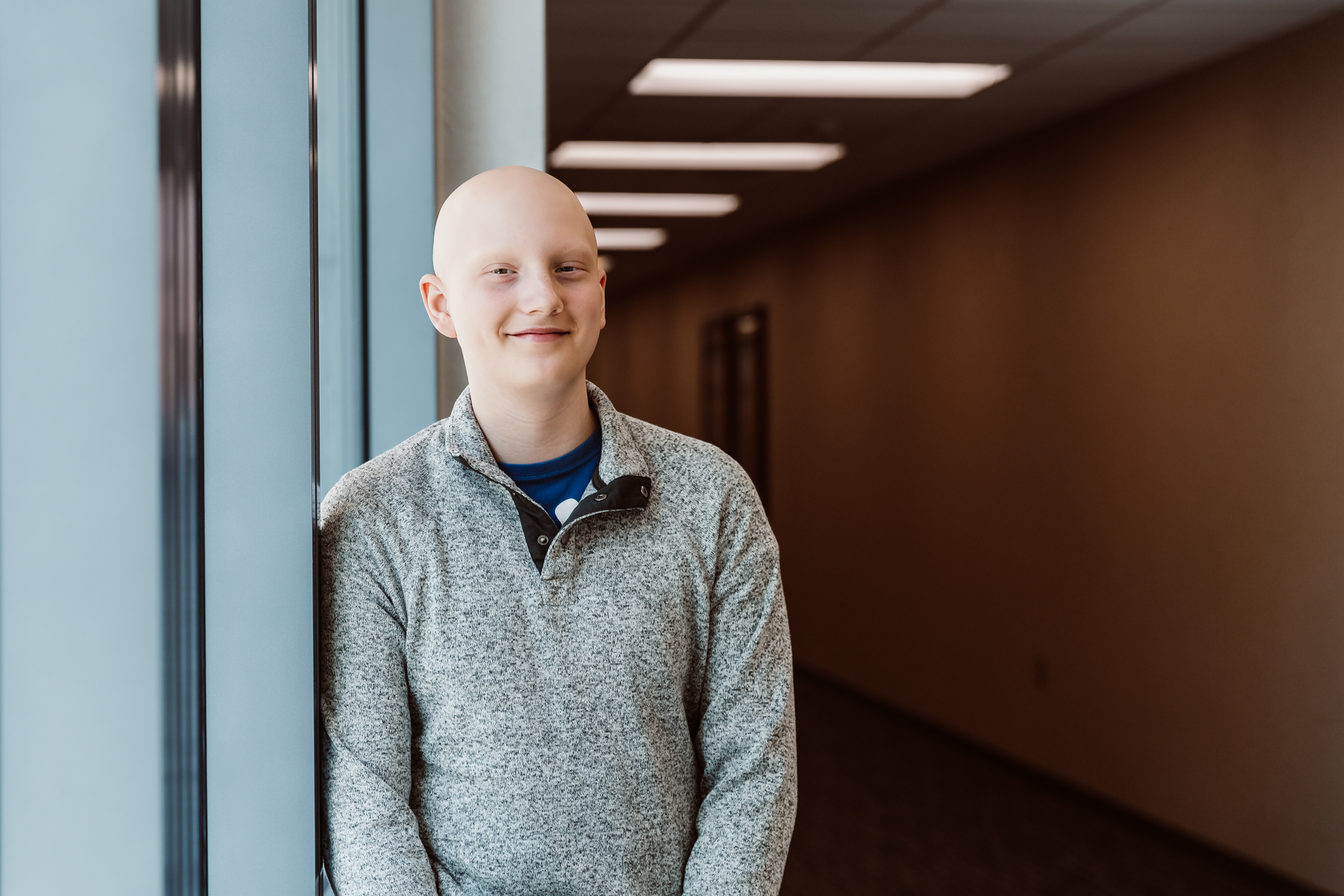
Bolton’s Bravery
With specialized, comprehensive care in hospitals tailored to the unique needs of pediatric patients, children’s hospitals help children and teens like Bolton defy the odds.

Every day, children’s hospitals help make moments possible. From providing access to the comprehensive care that children need to grow up to supporting children, teens, and their families with specialized treatment for some of the most complex illnesses. Discover more about the moments made possible by children’s hospital through patient stories from around the country.
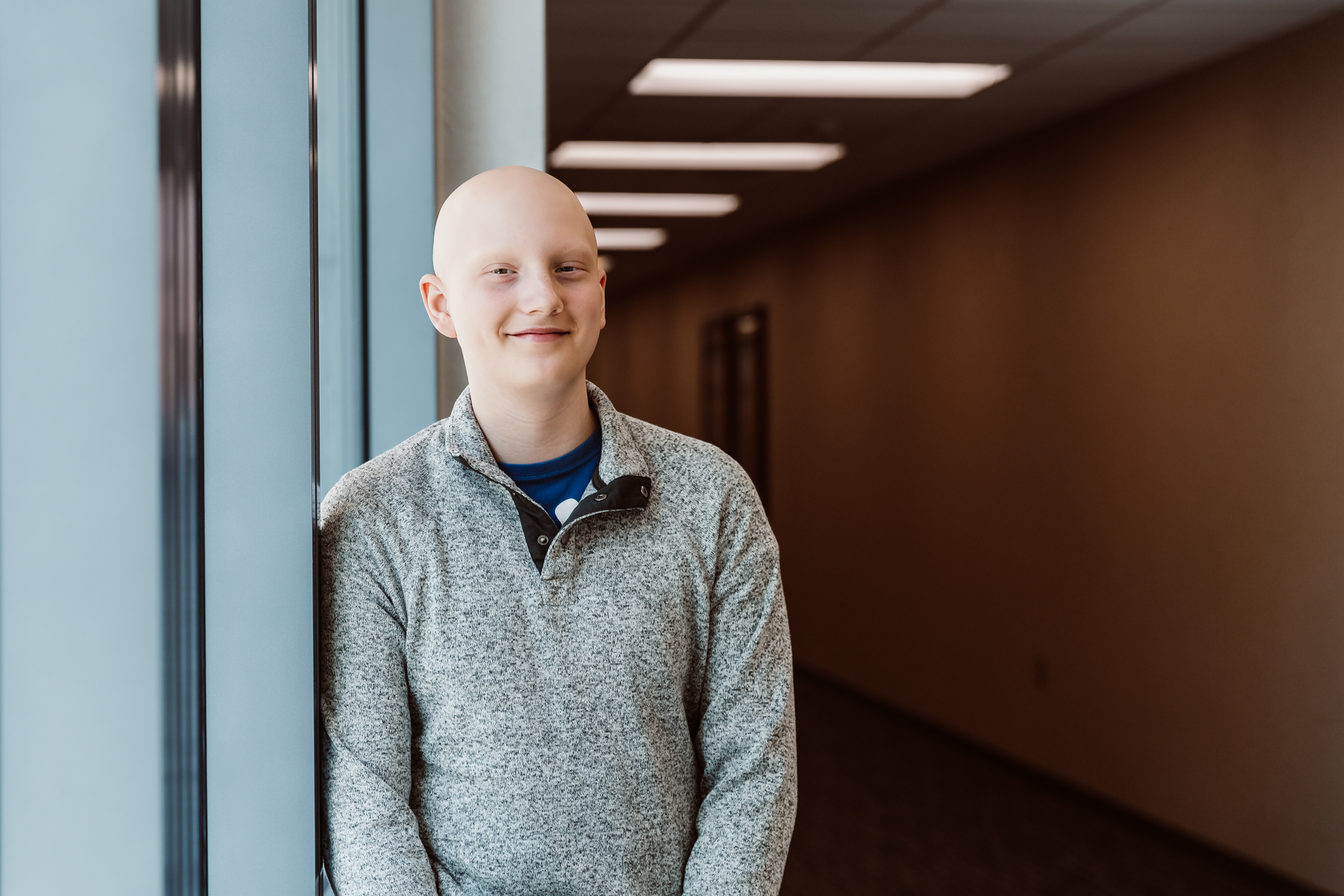
With specialized, comprehensive care in hospitals tailored to the unique needs of pediatric patients, children’s hospitals help children and teens like Bolton defy the odds.

Children’s hospitals provide advanced care for the most complex conditions in environments specially designed for pediatric patients, allowing children like Isaac to thrive.

The specialized multidisciplinary teams at children’s hospitals ensure that children and teens – like Cami – can beat multiple complex conditions like cancer and heart failure.

The advanced, specialized care that children’s hospitals provide make moments – like Joseph beating pediatric brain cancer – possible.

With care delivered by specially trained pediatric clinicians, in environments designed just for children, children’s hospitals help children and teens – like Daniella – navigate complex medical conditions.

When Sriansh was just three months old, his family grew concerned as he slept most of the day, arched his back, and could not control his eye movement. His parents brought him to Cincinnati Children’s, where he was diagnosed with AADC deficiency, a rare genetic disorder that disrupts dopamine and serotonin production in the brain. Sriansh’s family was told he might never walk, talk, or lift his head. But thanks to an experimental gene therapy clinical trial, his story took a groundbreaking turn. At just 16 months old, Sriansh became the youngest child in the world to receive a one-time gene therapy treatment, delivered directly into the brain through a minimally invasive surgical technique. His care team inserted an engineered virus carrying the missing gene, allowing his brain to begin producing the essential chemicals it lacked. Today, Sriansh is walking, running, and thriving because of this innovative clinical trial. This pioneering work helped lead to the first-ever FDA-approved gene therapy administered directly to the brain, offering hope for patients with rare genetic diseases once thought untreatable.

Biannka and Sakata Walker were overjoyed to learn they were expecting a baby through IVF. Despite a difficult pregnancy, Biannka stayed determined. At just 28 weeks, she was hospitalized, and baby Zion was born a month later while Sakata, who was deployed, watched from Afghanistan via video call. At age 3, Zion was diagnosed with cerebral palsy. After years of therapies, he became a candidate for the one-level laminectomy selective dorsal rhizotomy (SDR) surgery at Children’s Memorial Hermann Hospital—one of the few programs in the country offering this advanced procedure. SDR reduces the abnormal reflexes that cause muscle tightness in children with cerebral palsy. Just three months after surgery, Zion surprised his mom by standing on his own. Today, he’s running, jumping, and dancing—showing the remarkable impact of SDR and his family’s determination.

Baby Janelle’s cleft palate and recessed tongue made it difficult for her to get the nutrition she needed. Luckily, Bon Secours St. Mary’s Hospital’s cleft and craniofacial team was there to help. Janelle’s doctors created a personalized treatment plan to support her nutrition and prepare for surgical repair. But what made the biggest difference to her family was the compassion they received along the way. Doctors and nurses regularly called to check in, always celebrated small milestones, and ensured her parents never felt overwhelmed or alone. Janelle spent two weeks in the Neonatal Intensive Care Unit (NICU), where her care team supported her around the clock. Thanks to the Bon Secours Foundation, which helps families access essential healthcare regardless of financial barriers, Janelle’s hospital stay and surgery were made possible. Today, Janelle is back home, thriving under the care of her family. Her parents remain deeply grateful for the expert, loving care she received.

When baby Willow was born, everything seemed perfect. She was healthy and alert. Willow joined her big brother at home just a few days after she was born. But that first night home, something felt off—Willow was unusually sleepy, refusing to eat, and not wetting her diaper. Alarmed, Gina and her husband, Jarret, quickly sought medical care. Willow became unresponsive, and her local hospital wasn’t equipped to help her. That’s when the Norton Children’s “Just for Kids” Transport Team stepped in, transporting Willow to the NICU, where a multidisciplinary team worked tirelessly to uncover the cause of her critical condition. After testing, doctors discovered dangerously high ammonia levels caused by citrullinemia, a rare genetic disorder. Emergency dialysis stabilized Willow, and over time, she began to improve. Her journey continued with a successful liver transplant, made possible when Jarret became her living donor. Today, Willow is a thriving, joyful baby, smiling, growing, and meeting milestones every day.

Just weeks before 2-year-old Harlow was supposed to head to Jamaica to be the flower girl at her parents’ wedding, her mother noticed that her usually energetic daughter had developed a cough and grown lethargic. Her care team suggested she may have a mild viral infection and also suspected a heart murmur. But during the trip, Harlow’s condition began to worsen. The family flew her home and took her to UChicago Medicine Comer Children’s Hospital, where a blood test revealed she had a rare form of acute lymphoblastic leukemia, a cancer of the bone marrow and blood. As Harlow prepared for her inpatient stay at Comer Children’s, her family was comforted not only by her oncology team’s confidence but also by the investigative therapies and established treatments offered by leukemia specialists. Harlow’s smile never dimmed, and she remained resilient even when an uncommon chemo allergy required her to be intubated. Twenty-eight months later, she rang the bell to signify the end of her cancer treatment. Today, Harlow is a healthy 5-year-old who loves to cook with her family and watch “Family Feud.” Even better, she’s still smiling.

Before he was born, Nixon was diagnosed with spina bifida, a birth defect that can cause physical disability and developmental delays. His parents, Lindsey and Jared, were unsure what to do. They began researching hospitals and treatments to ensure the best future possible. In their search for care options, Nixon’s dad stumbled upon the CuRe trial, a clinical trial at UC Davis Children’s Hospital. The landmark trial is the world’s first in utero treatment for spina bifida, combining fetal surgery with stem cells to improve long-term outcomes before birth. The couple met with a medical team at UC Davis to learn more and decided to enroll in the trial right away. Throughout the trial, Lindsey and Jared felt deeply supported by their care team and grateful to be involved in such an innovative trial. A few months later, Nixon was born a healthy baby. To this day, he is making remarkable progress, walking and hitting cognitive, emotional and physical milestones.

At just 3 months old, Teresa survived severe burns from a tragic act of domestic violence. Now 14, she has spent most of her life not only recovering physically but channeling her healing into her passion for music. At Shriners Children’s Texas, she has found both the medical and emotional care she needs to thrive. Because most of Teresa’s injuries affected the tissue on her head, she didn’t have much hair in her early childhood. But through a multi-year series of tissue-expansion procedures on her scalp, Teresa will soon have a full head of hair, with one final procedure planned next year. Just as important, she’s found a way to heal her inner emotions through music. Working closely with the hospital’s music therapist in the child life department, Teresa writes songs, plays instruments, and records in the hospital’s very own studio, recently building the confidence to put on her first solo performance! Because of the medical care and unique music therapy Teresa receives at her children’s hospital, she is healing in every sense of the word.